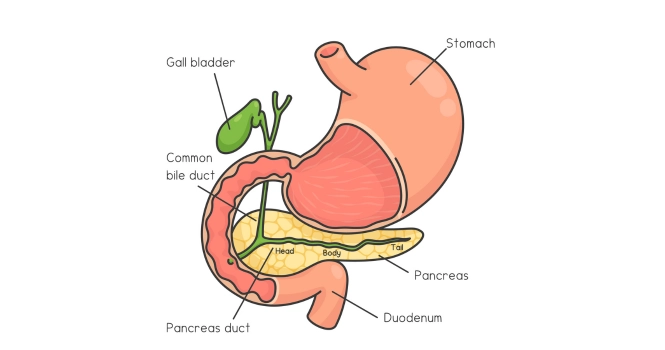
Gall Stones are hard deposits, like stones or pebbles, which vary in size, that form in the Gall bladder.
Gallbladder is a small organ beneath the Liver that stores bile.
What is the Medical Terms used for Gall Stones Disease?
Cholelithiasis, is the medical term for Gallstones, when found in Gallbladder.
The term “cholelithiasis” comes from the Greek words “chole” (bile), “lithos” (stone), and “iasis” (process or condition), literally translating to the condition of having bile stones.
Choledocholithiasis, is the medical term used when gallstones are found in Bile ducts.
The term itself breaks down into “choledocho-” referring to the common bile duct, “lith” meaning stone, and “iasis” signifying a condition or disease, so it translates roughly to “condition of having stones in the common bile duct.”
Cholecystitis is the medical term for inflammation of the gallbladder.
The term “cholecystitis” comes from the Greek words “chole” (bile), “kystis” (gallbladder), and “itis” (inflammation), which together translate to “inflammation of the gallbladder.”
Cholecystectomy is the medical term used for the surgical removal method of GallBladder. The term “cholecystectomy” comes from the Greek words “chole” (bile), “kystis” (gallbladder), and “ectomy” (removal), so it translates to “removal of the gallbladder.”
Cholangitis is an infection and inflammation of the bile duct system.
How are Gall Stones formed?
The formation of gall stones involves several processes within the gallbladder, which is a small organ that stores bile, a fluid produced by the liver to help digest fats.
This process occurs when substances in the bile start to crystallize.

Primarily, there are two types of gallstones:
- Cholesterol stones
- Pigment stones.
1. Cholesterol stones:
These are the most common type and are formed when the gallbladder isn’t able to empty effectively or when the bile contains more cholesterol than it can dissolve. When this happens, the excess cholesterol may start to crystallize and form stones.
2. Pigment stones:
These are less common and are formed when there’s an excess of bilirubin in the bile. Bilirubin is a byproduct of red blood cell breakdown, and conditions that lead to rapid cell breakdown can contribute to pigment stone formation. .
However, it’s important to note that many people with gallstones may not experience symptoms, and the stones may be discovered incidentally during routine medical procedures or imaging studies.
Treatment is generally recommended for symptomatic gallstones or in certain high-risk groups.
What are the Causes and Risk Factors of Gall Stones?
Several factors can contribute to gallstone formation,
Gender and age: Gallstones are more prevalent in women and older individuals.
Race and ethnicity: Certain ethnic groups, such as Mexican Americans and Native Americans, have higher rates of gall stone disease due to genetic factors.
Genetic predisposition: Specific genetic mutations can make individuals more susceptible to gallstones.
Weight and diet: Obesity, particularly in women, is a significant risk factor for gallstones. Diets high in carbohydrates and a high dietary glycemic load increase gallstone risk, while a diet high in fiber, fruits, and vegetables may decrease the risk.
Prolonged Fasting: Fasting for a prolonged period (over 5-10 days) can lead to the formation of biliary “sludge,” which can lead to gallstones or biliary symptoms.
Metabolic factors: Conditions such as diabetes mellitus, glucose intolerance, and insulin resistance can increase the risk of gallstone formation. Rapid weight loss and certain metabolic conditions can also contribute to the formation of gall stones.
Other medical conditions: Certain diseases, such as Crohn’s disease or conditions that cause liver cirrhosis and hepatitis C virus infection, can increase the risk of gallstones.
Medications: Some drugs, such as clofibrate, octreotide, and ceftriaxone, can increase the likelihood of gallstones.
What are Symptoms of Gall Stones?
While gallstones are common, not everyone who has them will experience symptoms. When symptoms do occur, they’re often a result of the gallstones interfering with the function of the gallbladder, liver, or pancreas.
The following are some symptoms that could indicate the presence of gallstones,
1. Biliary pain: The most common symptom of gallstones is a severe and sudden pain in the upper right part of the abdomen or the center of the abdomen, just below the breastbone.
This is known as biliary pain or gallbladder attack, which can last from 1 to 5 hours. The pain often occurs in the evening or at night, typically after a meal when the gallbladder is most active.
2. Back and shoulder pain: The pain may also radiate to the right shoulder or the back between the shoulder blades.
3. Nausea and vomiting: These symptoms often accompany the pain.
4. Jaundice: Yellowing of the skin and eyes, may occur if a gallstone exits the gallbladder and blocks the bile ducts leading to the liver.
5. Fever and chills: If a blockage leads to infection in the gallbladder (acute cholecystitis), you might develop a fever and chills.
6. Dark urine and light stools: If a gallstone blocks the bile ducts, bile can’t reach the intestines. Bile gives stool its brown color, so blockage could lead to lighter-colored stool and darker urine.
The frequency of these symptoms can vary. Some individuals might have gallbladder attacks once a month or less, while others might experience more frequent or prolonged attacks.
It’s essential to seek medical attention if you experience signs of a possible gallstone complication, such as intense pain, yellowing of the skin and eyes, or high fever with chills.
If persistent abdominal pain isn’t due to gallstones, it might be a hernia—learn more in our guide to [Hernia Surgery Explained…].
Prevalence of Gallstones
The following are the statistical data associated with gallstones,
1. General Prevalence: In the United States, the prevalence of gallstones was 8.6% in women and 5.5% in men.
2. Age: The incidence of gallstones increases with age, particularly in people over 60.
3. Ethnicity and Race: The rates of gallstones were higher in Mexican Americans compared to non-Hispanic whites and African Americans.
Over one third of individuals with sickle cell disease, a condition prevalent in the African American population, were likely to develop gallstones due to hemolysis.
Native Americans of both the Northern and Southern Hemispheres had high rates of cholesterol gallstones, possibly due to the presence of certain genes.
As many as 75% of Pima and other American Indian women over the age of 25 had gallstones.
4. Comorbidities: Gallstone disease was associated with increased overall mortality, cardiovascular mortality, and cancer mortality.
Diseases such as diabetes mellitus, glucose intolerance, and insulin resistance increased the risk of gallstones. A high intake of carbohydrate and high dietary glycemic load increased the risk of cholecystectomy in women.
The prevalence of gallbladder disease was increased in men (but not women) with cirrhosis and hepatitis C virus infection.
5. Diet and Lifestyle: Obesity, particularly in women, was a risk factor for gallstones. Rapid weight loss, as occurs after bariatric surgery, also increased the risk of symptomatic gallstone formation.
6. Medication and Other Factors: Certain drugs like clofibrate, octreotide, and ceftriaxone could cause gallstones.
Long-term fasting could lead to the formation of biliary “sludge,” which could further lead to gallstones or biliary symptoms.
Pregnancy, especially in obese women and those with insulin resistance, increased the risk of gallstones and symptomatic gallbladder disease.
Complications associated with Gall Stones
Gallstones can lead to several potential complications, often related to the blockage of the bile ducts. These include:
1. Acute Cholecystitis: This is inflammation of the gallbladder, usually due to a gallstone blocking the cystic duct. Symptoms can include severe and constant pain in the upper abdomen, fever, and sometimes jaundice. If left untreated, acute cholecystitis can lead to a perforated gallbladder, or even gallbladder gangrene.
2. Biliary Colic: This is severe abdominal pain caused by a temporary blockage of the bile duct. The pain usually comes on suddenly and quickly increases in intensity. It typically lasts 1 to 5 hours and can be accompanied by nausea and vomiting.
3. Cholangitis: This is an infection of the bile duct, which can cause fever, jaundice, and upper abdominal pain. This condition can be life-threatening and requires immediate treatment.
4. Gallstone Pancreatitis: A gallstone can block the pancreatic duct, leading to inflammation of the pancreas. This can cause severe abdominal pain and can be life-threatening.
5. Gallstone Ileus: This rare complication occurs when a large gallstone passes into the intestine and causes a blockage. This condition can lead to severe abdominal pain, vomiting, and constipation or diarrhea.
6. Increased Mortality: Gallstone disease is associated with increased overall mortality, cardiovascular mortality, and cancer mortality.
7. Liver Damage: If gallstones block the bile ducts for an extended period, they can lead to liver damage or liver failure.
8. Increased Risk of Certain Cancers: Gallstones have been reported to be associated with an increased risk of certain types of cancers, such as esophageal, proximal small intestinal, and colonic adenocarcinomas.
It’s important to note that while gallstones are common, not all will lead to these complications.
In fact, most people with gallstones do not have symptoms and do not need treatment.
However, in cases where gallstones cause symptoms or complications, treatment is usually necessary and may include medication, lifestyle changes, or surgery.
Diagnosis of Gallstones
Diagnosis of gallstones can be a straightforward process for a doctor given the right clinical context. The process can include the following steps:

1. Clinical History: In symptomatic patients, the doctor will inquire about the type and location of pain, its frequency and duration, and associated symptoms.
Gallstone symptoms, often referred to as biliary or “episodic gallbladder” pain, are typically characterized by pain in the upper right side of the abdomen or in the center of the abdomen below the breastbone.
This pain can last from 30 minutes to 24 hours, usually occurring in the evening or at night. There may be associated symptoms such as nausea or vomiting.
2. Physical Examination: The doctor will perform a physical exam to assess for tenderness in the abdomen, jaundice, or other signs of gallstones or complications thereof.
3. Blood Tests: These are not used to detect gallstones directly but can provide clues about any complications. For example, liver function tests can help identify blockages or infections in the bile ducts, and a complete blood count can indicate infection or inflammation in the body.
4. Imaging Tests: This is the most crucial step in the diagnosis of gallstones. An ultrasound of the abdomen is the first-line imaging test as it is safe, cost-effective, and has a high sensitivity for detecting gallstones.
Other imaging tests like computed tomography (CT), magnetic resonance imaging (MRI), and hepatobiliary iminodiacetic acid (HIDA) scans can be used when ultrasound findings are inconclusive or complications are suspected.
5. Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure can both diagnose and treat gallstones in the bile duct. It involves inserting a long, flexible tube (endoscope) down the throat, through the stomach, and into the upper part of the small intestine. A dye is injected through the tube into the bile ducts, which makes them visible on an X-ray.
Gallstones are frequently asymptomatic and can be discovered incidentally during a routine ultrasound study.
However, once diagnosed, monitoring or treatment may be necessary, depending on whether or not there are symptoms or complications.
Treatment Options for Gall Stones
The treatment options for gallstones primarily depend on whether or not they’re causing symptoms. In many cases, gallstones are asymptomatic and may not require any immediate treatment. However, if symptoms occur, the following treatment options may be considered:
1. Lifestyle Modifications: Diet changes can help manage symptoms of gallstones, especially in the early stages. This includes eating a healthy diet that’s low in fat and high in fiber, maintaining a healthy weight, and regularly exercising. Rapid weight loss should be avoided, as it can lead to gallstone formation.
2. Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as diclofenac, can be used to relieve biliary pain.
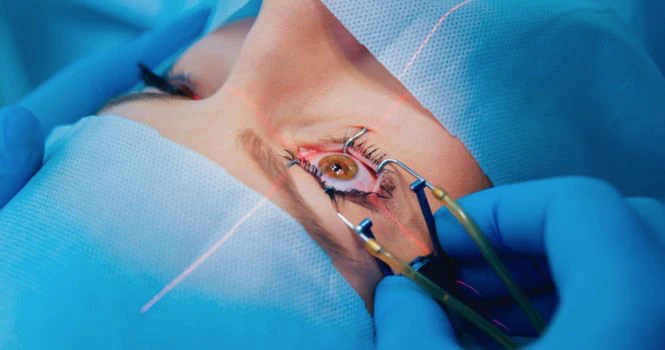
3. Laparoscopic Cholecystectomy: This is the treatment of choice for symptomatic gallbladder disease. It’s a type of surgery where the gallbladder is removed using a minimally invasive technique. Patients usually recover faster with this procedure than with traditional open surgery and often go home within one day of the operation.
4. Open Cholecystectomy: This traditional form of surgery may be necessary if complications arise during a laparoscopic cholecystectomy or if the patient has a severe gallbladder disease.
5. ERCP (Endoscopic Retrograde Cholangiopancreatography): This procedure can be used to remove stones in the bile duct. It’s not typically used for stones in the gallbladder itself.
6. Medication: In some selected cases, oral bile salt therapy, such as Ursodeoxycholic acid, can be used to dissolve cholesterol stones. However, this treatment can take up to 2 years, and gallstones can recur in half of the patients within 5 years, after treatment is stopped.
7. Lithotripsy: Although not generally used in the United States, lithotripsy can be used to break down single radiolucent stones smaller than 20 mm in diameter in combination with bile salt therapy.
As with all medical procedures, there are potential risks involved with gallstone treatments, such as infections, bleeding, and injuries to the bile duct.
Therefore, doctors will generally consider the overall health status of the patient, the severity of the symptoms, and the potential benefits versus the risks of treatment before deciding on the appropriate treatment course.
When is Surgery Indicated in Patients with Gallstones?
Surgery, specifically a cholecystectomy (removal of the gallbladder), is typically indicated in the following situations for patients with gallstones:
1. Symptomatic Gallstones: Gallstones that cause symptoms, such as biliary pain, are a common indication for surgery. This is because the presence of symptoms often suggests that gallstones are blocking the bile ducts, potentially leading to more serious complications like infection or inflammation.
2. Acute Cholecystitis: This is an inflammation of the gallbladder that occurs when a gallstone blocks the cystic duct. Acute cholecystitis often causes severe pain and fever, and is a common reason for emergency gallbladder removal.
3. Gallstone Pancreatitis: This is inflammation of the pancreas that occurs when a gallstone blocks the pancreatic duct. This condition can be severe or life-threatening, and often requires gallbladder removal once the pancreatitis has resolved.
4. Gallstone Ileus: This is a rare complication where a gallstone erodes into the digestive tract and causes an intestinal blockage. In these cases, an enterolithotomy (removal of the stone from the intestine) is often performed, and a cholecystectomy may be indicated.
5. Gallbladder Polyps or Stones larger than 3 cm: These may increase the risk of gallbladder cancer. Prophylactic cholecystectomy is generally recommended in these cases.
6. Chronic Cholecystitis or Biliary Dyskinesia: Chronic inflammation or abnormal motility of the gallbladder can lead to chronic abdominal pain. In these cases, a cholecystectomy may be recommended.
7. High-Risk Patients: In certain high-risk patients, such as those undergoing bariatric surgery or cardiac transplantation, or certain groups like Native Americans who are more prone to gallstone complications, prophylactic cholecystectomy may be considered.
It’s important to remember that the decision to proceed with surgery is always made on an individual basis, considering the patient’s specific symptoms, overall health, and personal preferences. The Doctors will thoroughly discuss the potential risks and benefits before making a final decision.
Prevention of Gallstones
Preventing gallstones can involve several lifestyle modifications, especially related to diet and regular health screenings. Here’s how these two aspects play a crucial role:
A. Diet and lifestyle modifications
1. Healthy Weight: Maintaining a healthy weight can help prevent gallstones. However, it’s important to lose weight gradually, as rapid weight loss can increase the risk of gallstones.
2. Balanced Diet: Eating a diet high in fiber, fruits, vegetables, and healthy fats can reduce the risk of gallstones. A diet that is low in fat, sugar, and refined carbohydrates is also beneficial.
3. Physical Activity: Regular physical activity can help maintain a healthy weight and lower the risk of gallstones.
4. Coffee: Consumption of caffeinated coffee has been shown to protect against gallstones in women.
5. Alcohol: Moderate consumption of alcohol has been linked with a decreased risk of gallstones.
6. Hydration: Drinking enough water can also help prevent gallstones by keeping the bile in the gallbladder fluid.
B. Regular Check-ups and Screenings for At-risk Individuals
Routine health screenings can play a crucial role in the early detection and prevention of gallstones, especially in individuals who are at a higher risk. These at-risk groups include:
1. Age: People over the age of 40, especially women, are more likely to develop gallstones.
2. Race: Certain ethnic groups, like Native Americans and Mexican Americans, are at a higher risk.
3. Family History: Those with a family history of gallstones are more likely to develop them.
4. Other Health Conditions: Individuals with conditions such as obesity, diabetes, cirrhosis, or certain blood disorders like sickle cell anemia are at increased risk.
5. Pregnancy: Pregnancy increases the risk of gallstones, and so pregnant women, particularly those who are obese or have insulin resistance, should be monitored closely.
Regular health check-ups allow doctors to assess these risk factors and provide early treatment options if necessary. They might also give advice on lifestyle changes to those who are at an increased risk.