Breast Enlargement is a topic that elicits a variety of responses from different people, ranging from empowerment and newfound confidence to questions about the societal pressures that might prompt someone to consider such a procedure.
The topic of breast enlargement is sensitive and personal. There are various reasons why individuals opt for this surgical procedure.
For some, it may be a way to restore breast volume lost after pregnancy or weight loss, for others, it may be a reconstructive option after mastectomy due to breast cancer. There are also those who choose breast enlargement for cosmetic purposes to enhance their overall appearance and confidence.
While this guide aims to provide a comprehensive overview, it is crucial to remember that every individual’s needs, motivations, and outcomes can be unique. Therefore, we encourage anyone considering breast enlargement to consult qualified medical professionals for personalized advice.
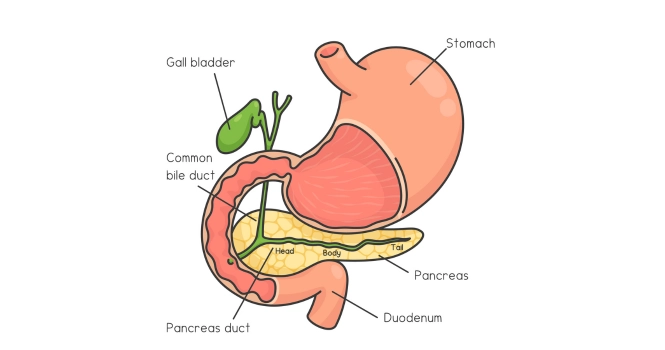
Let’s look into Surgical Methods,
Surgical Methods of Breast Enlargement
A. Silicone Implants
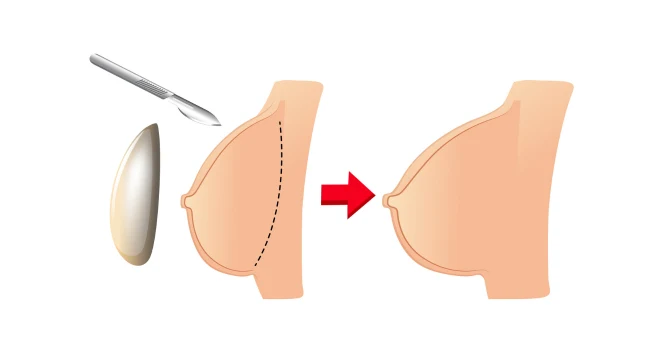
When it comes to breast enlargement, one of the most common methods involves the use of silicone implants. Silicone gel-filled implants have been in use for several decades and have undergone rigorous scientific evaluations. They are favored by many due to their natural feel and aesthetic appeal. This section aims to provide an in-depth look at silicone implants as a surgical option, covering various aspects such as the types available, the procedure itself, benefits, risks, and post-operative care.

Types of Silicone Implants
Silicone implants come in various shapes, sizes, and textures to cater to individual needs and preferences.
The two primary shapes are:
Round Implants: These are the most commonly used and tend to give the breast a fuller appearance.
Anatomical or ‘Teardrop’ Implants: These are designed to mimic the natural slope of the breast and are often chosen for a more ‘natural’ look.
Silicone implants may also differ in their outer shell, which can be either smooth or textured.
The Procedure
The silicone implant surgery is generally performed under general anesthesia and takes approximately one to two hours. Here’s a simplified step-by-step overview:
Incision: The surgeon makes an incision, commonly under the breast, around the areola, or in the armpit, depending on various factors like your anatomy, the type of implant, and how much enlargement is involved.
Insertion and Placement: The silicone implant is then inserted either behind the breast tissue or beneath the chest muscle.
Closure: Once the implant is properly positioned, the incisions are closed using sutures, surgical tape, or adhesive.
Benefits
- Natural Feel: Many women report that silicone implants feel more like natural breast tissue compared to other types of implants.
- Less Rippling: Silicone implants tend to have less visible rippling or wrinkling.
Risks and Considerations
Like any surgical procedure, silicone implant surgery comes with its own set of risks, such as:
- Capsular Contracture: This occurs when the scar tissue around the implant hardens, which may require additional surgery to correct.
- Rupture: While modern silicone implants are highly durable, there’s still a risk of rupture over time.
- Anesthesia Risks: As the surgery is usually performed under general anesthesia, there are associated risks.
It is also essential to note that silicone implants require regular monitoring via MRI or ultrasound to check the implant’s integrity, as a rupture may be “silent,” meaning it doesn’t present immediate symptoms.
Post-Operative Care
After the procedure, you’ll likely experience soreness, swelling, and bruising, for which pain medication and supportive garments will be prescribed. Follow-up appointments are crucial for monitoring healing and for any early signs of complications.
Choosing to undergo breast enlargement is a deeply personal decision, and being well-informed is crucial.
If you’re considering silicone implants, consult with a board-certified plastic surgeon who specializes in breast enlargement to discuss whether this option is suitable for your needs and expectations.
B. Saline Implants
Another widely-used option for breast augmentation is saline implants. Composed of a silicone outer shell filled with sterile saline solution (salt water), these implants offer a different set of advantages and drawbacks compared to their silicone counterparts.
This section will delve into the specifics of saline implants, covering topics like types, the surgical procedure, benefits, risks, and aftercare.
Types of Saline Implants
Saline implants primarily come in two shapes:
Round Implants: These are spherical and can provide a fuller appearance to the upper portion of the breast.
Contoured Implants: Also known as anatomical or ‘teardrop’ implants, these aim to provide a more natural-looking breast contour.
Both types can have either a smooth or textured outer shell, depending on your needs and your surgeon’s recommendations.
The Procedure
The surgery for inserting saline implants is quite similar to that for silicone implants:
Incision: The surgeon makes an incision, usually either under the breast, around the areola, or in the armpit.
Insertion and Placement: An empty implant shell is inserted into the pocket created either behind the breast tissue or beneath the chest muscle.
Filling: The implant is then filled with sterile saline to the predetermined size.
Closure: The incisions are sealed using sutures, surgical tape, or adhesive.
Benefits
- Adjustable Size: One key advantage of saline implants is that they are filled after being inserted, allowing for minor adjustments in size during surgery.
- Smaller Incision: Since the implant is inserted empty and then filled, the required incision is generally smaller.
- Visible Leak Detection: In the event of a rupture, the saline solution is safely absorbed by the body, and the leak is immediately noticeable due to visible deflation of the implant.
Risks and Considerations
Saline implants also come with specific risks:
- Capsular Contracture: Like silicone implants, saline implants can lead to the formation of tight scar tissue around the implant.
- Rippling: Saline implants are more prone to visible wrinkling or rippling.
- Less Natural Feel: Some people find that saline implants don’t feel as natural as silicone implants.
Post-Operative Care
Post-operative care is similar to that of silicone implants. You’ll likely be prescribed pain medication and may need to wear a surgical bra or compression garments.
Monitoring through regular check-ups is crucial to ensure that the implants are in good condition and to promptly address any complications.
As with any surgical procedure, especially one that is as personal and life-changing as breast enlargement, it is crucial to consult a qualified, board-certified plastic surgeon to discuss your options, expectations, and concerns.
Saline implants might be the right choice for some people based on their individual needs, body type, and the results they wish to achieve.
C. Gummy Bear Implants
In the evolving landscape of breast enlargement, gummy bear implants have emerged as an option that combines the best of both worlds: the durability of silicone and a shape that mimics natural breast tissue.
Officially known as “form-stable” or “cohesive silicone gel implants,” they have earned the nickname “gummy bear” due to their consistency, which is similar to the popular chewy candies.
In this section, we will explore the nuances of gummy bear implants, including their types, the surgical procedure, benefits, risks, and what to expect post-operatively.
Types of Gummy Bear Implants
Gummy bear implants are available mainly in the ‘teardrop’ or anatomical shape, which aims to mimic the natural slope of the breast. They maintain their shape due to the cohesive silicone gel inside, making them less likely to fold, ripple, or rupture.
The Procedure
The steps involved in inserting gummy bear implants are similar to other implant types:
Incision: An incision is made, usually under the breast, around the areola, or less commonly, in the armpit.
Insertion and Placement: The implant is inserted either behind the breast tissue or beneath the chest muscle.
Closure: The incisions are then closed with sutures, surgical tape, or adhesive.
However, because gummy bear implants are shaped, it’s crucial for the surgeon to place them with precision to ensure they align correctly and do not rotate post-surgery.
Benefits
- Natural Look and Feel: These implants are often touted for their natural appearance and texture.
- Reduced Risk of Rippling: The consistency of the gel inside makes them less likely to wrinkle or ripple.
- Stable Form: Unlike other implants, they hold their shape over time, reducing the risk of aesthetic issues linked to shifting or deformation.
Risks and Considerations
Despite their benefits, gummy bear implants have their own set of risks:
- Potential for Rotation: Because these implants are shaped rather than round, there is a risk they could rotate, creating an abnormal appearance that may require corrective surgery.
- Larger Incisions: Due to their form-stable nature, these implants typically require larger incisions, which could lead to more visible scarring.
- Cost: Gummy bear implants tend to be more expensive than their saline or traditional silicone counterparts.
Post-Operative Care
The recovery process for gummy bear implants is comparable to other types of implants, involving pain medication, supportive garments, and regular follow-up appointments for monitoring.
Due to the potential for implant rotation, some surgeons may recommend specific exercises or precautions during the recovery period.
As always, choosing the right type of breast implant is a highly personal decision that should be made in consultation with a qualified, board-certified plastic surgeon.
This ensures that you are aware of all the options, risks, and benefits, and that the implant you choose aligns with your aesthetic goals and lifestyle.
D. Fat Transfer for Breast Enlargement

Fat transfer, also known as autologous fat grafting or lipomodelling, is a breast enlargement method that has gained popularity as a more “natural” alternative to traditional implants.
This procedure involves harvesting fat from one area of the patient’s body and then injecting it into the breasts. In this section, we’ll explore the specifics of fat transfer, including the procedure itself, benefits, risks, and what to expect during the post-operative period.
The Procedure
The fat transfer procedure can be broken down into the following main steps:
Fat Harvesting: Fat cells are extracted from another part of the body—commonly the abdomen, thighs, or flanks—using liposuction.
Preparation: The harvested fat is then purified to isolate the fat cells from other tissues.
Injection: The purified fat cells are meticulously injected into different areas of the breast to achieve the desired size and shape.
Closure: Typically, the incisions required for both liposuction and fat injection are small and are closed with sutures.
Benefits
- Natural Material: Because the procedure uses your own body fat, there is no risk of allergic reaction or implant rejection.
- Dual Benefit: The procedure offers the advantage of contouring the area from which the fat is harvested.
- Minimal Scarring: Smaller incisions mean less noticeable scarring.
- Natural Feel: Many patients report that their breasts feel and appear more natural post-procedure.
Risks and Considerations
Although fat transfer has its perks, there are also risks and limitations:
- Limited enlargement: The degree to which you can increase your breast size is limited compared to traditional implants.
- Fat Absorption: Over time, some of the transferred fat may be reabsorbed by the body, which could reduce the initial size increase and potentially require additional procedures.
- Calcification: There’s a risk that the transferred fat could calcify and complicate mammography readings.
- Surgical Risks: Like any surgery, this procedure comes with risks like infection, scarring, and anesthesia complications.
Post-Operative Care
Post-operative care following a fat transfer is twofold:
Breast Area: Mild to moderate swelling and bruising are to be expected. A support bra may be recommended to help shape the breasts and minimize swelling.
Donor Area: The area from which fat was harvested will also require care. You may need to wear compression garments and avoid strenuous activity.
Regular follow-ups will be necessary to monitor the healing process, the state of the transferred fat, and to assess the aesthetic results.
Consultation with a board-certified plastic surgeon experienced in fat transfer procedures is essential for determining whether this technique is appropriate for you.
Be sure to discuss your aesthetic goals, medical history, and any concerns you may have to arrive at an informed and personalized decision.
Position and Placement of Implant for Breast Augmentation
A. Subglandular Placement
When it comes to breast enlargement, the placement of the implant is a crucial factor that can significantly impact the final result.
One common option for implant placement is the subglandular method, also known as “above the muscle” or “over the muscle” placement. In this approach, the implant is positioned between the breast tissue and the pectoral muscle.
This section will explore the specifics of subglandular placement, including what the procedure entails, its benefits, risks, and considerations for post-operative care.
The Procedure
Here is a simplified outline of how the subglandular placement generally occurs:
Incision: An incision is made in a location determined by your anatomy and surgeon’s recommendation—commonly under the breast, around the areola, or in the armpit.
Creating the Pocket: A pocket is carefully created between the breast tissue and the pectoral muscle to accommodate the implant.
Insertion: The implant (silicone, saline, or gummy bear) is then inserted into this pocket.
Closure: The incisions are closed using sutures, surgical tape, or adhesive.
Benefits
- Less Postoperative Pain: As the pectoral muscle is not disturbed, many patients report less postoperative pain compared to submuscular (below the muscle) placements.
- Quicker Recovery: The healing time is generally faster, allowing for a quicker return to physical activity.
- Natural Movement: Subglandular placement can result in more natural breast movement as the implant is not positioned under the muscle, which contracts during physical activity.
- Better for Athletes: For women who engage in high levels of chest muscle activity, subglandular placement may be more suitable.
Risks and Considerations
- Visibility and Palpability: In thinner women with less natural breast tissue, the implant might be more visible or palpable under the skin.
- Capsular Contracture: Some studies suggest a higher likelihood of capsular contracture (scar tissue hardening around the implant) with subglandular placement compared to submuscular placement.
- Interference with Mammography: Because the implant is closer to the breast tissue, it might create challenges in breast imaging, although advanced imaging techniques can often mitigate this issue.
Post-Operative Care
After the procedure, you may be prescribed medication to manage pain and inflammation.
A surgical or support bra is often recommended to help shape the breasts and minimize swelling. As the muscle tissue is less impacted, recovery may be quicker, but it’s still essential to adhere to your surgeon’s guidance on resuming physical activities.
Subglandular placement may not be suitable for everyone. The right implant placement for you will depend on multiple factors, including your body type, lifestyle, the amount of natural breast tissue you have, and your aesthetic goals.
As always, a detailed consultation with a board-certified plastic surgeon is crucial for making an informed decision about breast enlargement and implant placement.
B. Submuscular Placement
Submuscular placement, also commonly referred to as “under the muscle” or “below the muscle” placement, is another popular option in breast enlargement surgeries.
In this method, the implant is positioned beneath the pectoral muscle, partially covered by it. This section will provide an overview of submuscular placement, discussing the procedure, its benefits, associated risks, and guidelines for post-operative care.
The Procedure
The steps for submuscular placement are generally as follows:
- Incision: Similar to subglandular placement, an incision is made either under the breast, around the areola, or in the armpit.
- Creating the Pocket: A pocket is formed underneath the pectoral muscle to accommodate the implant.
- Insertion: The chosen implant (silicone, saline, or gummy bear) is then inserted into the pocket.
- Closure: The incisions are sealed with sutures, surgical tape, or adhesive.
Benefits
- Natural Appearance: This method can offer a more natural look, especially in women with less existing breast tissue, as the muscle layer can camouflage the implant.
- Lower Risk of Capsular Contracture: Submuscular placement has been associated with a slightly lower risk of capsular contracture compared to subglandular placement.
- Improved Imaging: Having the implant below the muscle may interfere less with mammographic imaging.
Risks and Considerations
- More Postoperative Pain: As the procedure involves manipulating the muscle, you may experience more discomfort during the initial recovery period.
- Longer Recovery Time: Healing and return to regular activities may take longer compared to the subglandular method.
- Animation Deformity: In some cases, muscle contraction can cause the implant to shift, sometimes referred to as “animation deformity.”
Post-Operative Care
Post-operative care usually involves:
- Pain Management: You’ll likely be prescribed pain medication, and perhaps muscle relaxants, to help manage discomfort.
- Support Garments: A surgical or support bra is generally recommended to support the breasts and minimize swelling.
- Activity Restrictions: Your surgeon will guide you on when you can safely return to daily activities and exercise, keeping in mind that recovery may take longer than with subglandular placement.
Choosing between subglandular and submuscular placement is a complex decision that depends on various factors, such as your body type, the amount of natural breast tissue, your lifestyle, and what you hope to achieve aesthetically.
As always, consulting with a qualified, board-certified plastic surgeon is essential to making an informed decision that is best suited to your individual needs and goals.
C. Subfascial Placement
Subfascial placement is a less commonly discussed but increasingly popular method for breast implant placement. In this technique, the implant is positioned under the fascia but above the pectoral muscle.
The fascia is a thin layer of connective tissue that covers muscles and other internal structures. This section aims to shed light on the specifics of subfascial placement, from the procedure itself to its advantages, risks, and the post-operative care regimen.
The Procedure
Here’s a simplified step-by-step guide to subfascial placement:
- Incision: An incision is typically made either under the breast (inframammary), around the areola (periareolar), or in the armpit (transaxillary).
- Creating the Pocket: A pocket is meticulously created underneath the fascial layer but above the pectoral muscle.
- Insertion: The implant (silicone, saline, or gummy bear) is inserted into this newly created pocket.
- Closure: The incisions are closed using sutures, surgical tape, or adhesive.
Benefits
- Aesthetic Appeal: The fascial layer provides additional support and coverage for the implant, which can result in a more natural look.
- Less Pain: Because the pectoral muscle is not manipulated, patients often experience less postoperative pain compared to submuscular placement.
- Shorter Recovery Time: Similar to subglandular placement, the recovery period is generally shorter.
- Reduced Risk of Animation Deformity: Unlike submuscular placement, there’s a lower risk of animation deformity since the muscle remains untouched.
Risks and Considerations
- Visibility and Palpability: In women with thin skin and little breast tissue, the implant may still be more palpable compared to submuscular placement.
- Capsular Contracture: The risk factors for capsular contracture with subfascial placement are still the subject of medical research, but some studies suggest it may be closer to subglandular than submuscular in this regard.
- Limited Studies: There are fewer long-term studies on subfascial placement compared to the more traditional methods, which means that some risks may not be fully understood yet.
Post-Operative Care
- Pain Management: Mild to moderate pain can be managed with prescribed medications.
- Support Garments: A surgical or support bra is often advised to help shape the breasts and minimize swelling.
- Follow-Up Appointments: Regular check-ups will be essential to monitor the implant placement, healing, and any potential complications.
Subfascial placement can be a suitable middle ground for those who want some of the benefits of both subglandular and submuscular placements.
However, it’s vital to consult with a board-certified plastic surgeon experienced in this particular technique to discuss if it’s the best option for you.
Your anatomy, lifestyle, and aesthetic goals will all factor into whether subfascial placement is the most appropriate choice for your breast enlargement.
D. Dual Plane Placement
In the realm of breast enlargement, dual plane placement represents a hybrid approach that aims to capitalize on the advantages of both submuscular and subglandular placements.
In this technique, the implant is partially placed beneath the pectoral muscle at the upper pole, while the lower pole remains beneath the breast tissue but above the muscle. This section will delve into the specifics of dual plane placement, covering the procedure, its benefits, associated risks, and post-operative care recommendations.
The Procedure
The dual plane breast enlargement typically involves the following steps:
- Incision: As with other methods, an incision is made either in the inframammary fold, around the areola, or in the armpit.
- Creating the Pocket: A specialized pocket is formed that allows for a dual-plane placement of the implant. The upper part of the pocket is beneath the pectoral muscle, and the lower part is above the muscle but under the glandular tissue.
- Insertion: The selected implant (silicone, saline, or gummy bear) is inserted into this dual-plane pocket.
- Closure: Incisions are closed using sutures, surgical tape, or adhesive.
Benefits
- Natural Appearance: This method often results in a very natural-looking breast shape, as it combines the benefits of muscle coverage at the top with a natural droop at the bottom.
- Versatility: Particularly useful for patients with mild to moderate breast sagging (ptosis) or those who have thin skin but still want the benefits of muscle coverage.
- Reduced Risk of Complications: Dual plane placement can offer a reduced risk of complications like implant visibility and rippling.
Risks and Considerations
- Complexity: The procedure can be more complex and may require a highly skilled surgeon experienced in dual plane techniques.
- Postoperative Pain: While generally less than with complete submuscular placement, some postoperative pain should be expected due to muscle manipulation.
- Longer Recovery Time: Recovery might be slightly longer than with subglandular placement but is often shorter than full submuscular placement.
Post-Operative Care
- Pain Management: Prescription medications are commonly provided to manage post-surgical discomfort.
- Support Garments: A surgical bra is usually recommended to help support the breasts and minimize swelling.
- Activity Restrictions: Exercise and strenuous activity will be restricted for a specific period, as advised by your surgeon.
- Follow-up: Regular post-operative visits will be scheduled to monitor healing, implant position, and to identify any potential complications early on.
Choosing the right implant placement is a highly individualized decision that should be made in consultation with a qualified, board-certified plastic surgeon.
Dual plane placement can be an excellent option for those who wish to combine the benefits of submuscular and subglandular placements, but it’s important to have a comprehensive evaluation to determine if this technique is appropriate for your specific needs and aesthetic goals.
Incision Types for Breast Enlargement
One of the key decisions in breast enlargement surgery is the type of incision that will be used to insert the implant.
This choice can influence not only the scarring but also potential complications and even the type of implant that can be used. Below, we delve into the most commonly employed incision types: Inframammary, Periareolar, Transaxillary, and Transumbilical.
A. Inframammary Incision
- Description: The inframammary incision is made along the crease beneath the breast, known as the inframammary fold.
- Advantages:
- Allows for precise placement of the implant.
- Suitable for all types of implants.
- The scar is generally well-hidden beneath the breast.
- Risks and Considerations:
- The incision is close to the breast, which may slightly increase the risk of infection.
- Post-Operative Care: Scar creams or silicone gel strips can be used to minimize scarring.
B. Periareolar Incision
- Description: This incision is made around the border of the areola, the pigmented area surrounding the nipple.
- Advantages:
- The scar is often well-concealed due to the color transition between the areola and the surrounding breast skin.
- Suitable for smaller implants.
- Risks and Considerations:
- May interfere with future breastfeeding or nipple sensation.
- Higher risk of capsular contracture compared to other incision types.
- Post-Operative Care: Extra caution may be required to prevent infection around the nipple area.
C. Transaxillary Incision
- Description: The transaxillary incision is made in the armpit, and a tunnel is created to the breast area for implant placement.
- Advantages:
- No scarring on the breast itself.
- Suitable for saline implants that can be filled after placement.
- Risks and Considerations:
- The scar may be visible when wearing sleeveless clothing.
- Some surgeons find it challenging to achieve precise implant positioning through this method.
- Post-Operative Care: Scarring can be treated with topical creams; however, scarring in the armpit may be more visible depending on skin type and healing.
D. Transumbilical Incision (TUBA)
- Description: An incision is made in the navel, and the implant is inserted through a tunnel up to the breast.
- Advantages:
- No scarring on the breasts.
- Less invasive, often resulting in quicker recovery.
- Risks and Considerations:
- Typically only possible for saline implants.
- Implant positioning may be less precise.
- Fewer surgeons are skilled in this technique.
- Post-Operative Care: Due to the distance from the breast, risk of infection is often considered lower, but proper care is still required.
Each incision type has its own set of advantages and disadvantages, and the best option for you will depend on several factors, such as the type of implant, your anatomy, and your personal preferences.
It’s crucial to have a thorough discussion with a board-certified plastic surgeon to determine which incision type is best suited for your specific needs and aesthetic goals.
Non-Surgical Methods for Breast Enlargement
While surgical methods for breast augmentation remain popular and are generally more permanent, there is a growing interest in less invasive, non-surgical options.
These alternative treatments can offer subtle changes without the need for general anesthesia, incisions, or extensive downtime.
Here, we discuss some non-surgical methods, including Hyaluronic Acid Fillers, Sculptra, PRP (Platelet-Rich Plasma) Injections, and Hormone Therapy.
A. Hyaluronic Acid Fillers
- Description: Hyaluronic acid is a natural substance found in the body, commonly used for facial fillers. For breast enhancement, it can be injected to increase volume temporarily.
- Advantages:
- Quick procedures are often completed in under an hour.
- Immediate results.
- No downtime.
- Risks and Considerations:
- Results are temporary, usually lasting 6 to 12 months.
- High costs for maintenance.
- Risk of unevenness or lumpiness.
- Post-Treatment Care: Minimal; some patients may experience bruising or swelling, which generally resolves quickly.
B. Sculptra
- Description: Sculptra is a biocompatible, biodegradable synthetic material known as poly-L-lactic acid, used to add volume over time.
- Advantages:
- Results can last up to 2 years.
- Gradual increase in size allows for more natural adaptation.
- Risks and Considerations:
- Multiple treatments may be required for desired results.
- Risk of nodules or lumps.
- Post-Treatment Care: Massaging the area is often recommended to distribute the material evenly.
C. PRP (Platelet-Rich Plasma) Injections
- Description: PRP involves extracting a patient’s own blood, processing it to concentrate the platelets, and then injecting it back into the breast tissue to stimulate growth.
- Advantages:
- Utilizes the body’s natural materials.
- May improve skin texture and integrity.
- Risks and Considerations:
- Results are very subtle and may require multiple treatments.
- Not suitable for significant enlargement.
- Post-Treatment Care: Minimal downtime, but some bruising or swelling may occur.
D. Hormone Therapy
- Description: Hormone therapy involves the use of hormones like estrogen to stimulate breast growth.
- Advantages:
- May offer more natural-looking results over time.
- Can be part of a broader hormone replacement therapy plan.
- Risks and Considerations:
- Slow process requiring ongoing treatment.
- Potential side effects including weight gain, mood changes, and increased risk of certain cancers.
- Not recommended for those with a history of hormone-sensitive cancers.
- Post-Treatment Care: Ongoing medical monitoring is essential.
As with any medical procedure, it’s crucial to consult healthcare providers for a comprehensive understanding of your options, potential risks, and expected outcomes.
Non-surgical methods often involve ongoing treatments and maintenance, and the results are generally less dramatic compared to surgical methods. Make sure to consult a qualified medical professional to determine which method is most appropriate for your specific needs and goals.