Piles, also known as hemorrhoids, are a common concern that affects a large number of people from various walks of life.
When conservative treatments like dietary adjustments and medications fall short, surgery becomes a necessary and effective option.
In India, piles surgery has evolved significantly, with a variety of minimally invasive procedures now available, offering shorter recovery times and less discomfort than traditional surgeries.
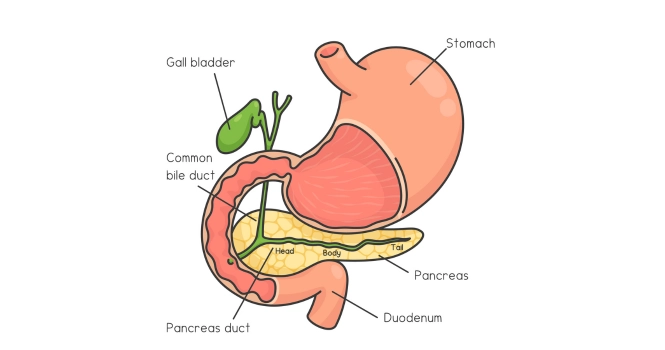
Before going into details, Let’s understand some basics
What are Piles?
Definition and Types
Piles, commonly known as hemorrhoids, are swollen veins in the rectum and anus that can cause discomfort and bleeding.
It’s also called in other local languages as in,
- Kannada: ಮೂಲವ್ಯಾಧಿ (pronounced as Mūlavādhi)
- Hindi: बवासीर (pronounced as Bavāsīr)
- Spanish: Hemorroides
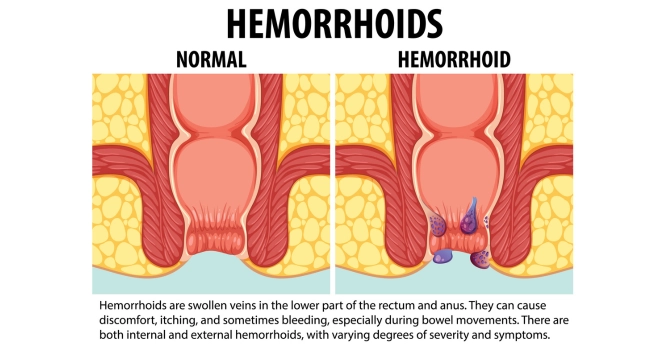
Hemorrhoids are primarily classified into two types:
1. Internal Hemorrhoids: These occur inside the rectum and are usually not visible or felt. Straining or irritation when passing stool can cause painless bleeding during bowel movements. In some cases, internal hemorrhoids can prolapse or extend outside the anal opening, leading to more noticeable symptoms and discomfort.
2. External Hemorrhoids: These form under the skin around the anus and are where most of the discomfort associated with hemorrhoids occurs. They can be felt when cleaning the anal area and might cause itching, bleeding, and swelling.
Causes and Symptoms

The exact cause of piles is not entirely understood but several factors contribute to their development:
- Straining during bowel movements
- Chronic constipation or diarrhea
- A low-fiber diet
- Prolonged sitting, especially on the toilet
- Aging, as the tissues supporting the veins in the rectum and anus can weaken and stretch
- Pregnancy, due to the pressure of the growing uterus and hormonal changes
- Obesity
- Genetic predisposition
Symptoms of piles vary depending on whether they are internal or external but can include:
- Painless bleeding during bowel movements – You might notice small amounts of bright red blood on your toilet tissue or in the toilet.
- Itching or irritation in the anal region
- Pain or discomfort, especially when sitting
- Swelling around the anus
- A lump near your anus, which may be sensitive or painful
- Leakage of feces
In some cases, symptoms can signify more serious conditions, like colorectal cancer.
Therefore, it’s essential to consult a doctor if experiencing any of these symptoms, especially if they persist or worsen over time.
Early diagnosis and treatment can help manage symptoms and prevent complications such as anemia from chronic blood loss, strangulated hemorrhoids, and chronic incontinence.
When is Surgery Necessary?
Indications for Surgery
While many cases of piles can be managed with lifestyle changes, over-the-counter treatments, or minimally invasive office procedures, there are certain situations where surgery becomes necessary:
1. Severe or Persistent Symptoms: If hemorrhoids cause severe pain, extensive bleeding, or persist despite conservative treatments, surgery may be the best option.
2. Large External Hemorrhoids: Large, external hemorrhoids that do not respond to other treatments may require surgical removal.
3. Prolapsed Internal Hemorrhoids: Internal hemorrhoids that have prolapsed (i.e., extended outside the anal canal) and cannot be manually repositioned may necessitate surgical intervention.
4. Complications: In cases where hemorrhoids lead to significant complications like anemia from chronic blood loss or if there is a suspicion of strangulation (where the blood supply to the hemorrhoid is cut off), surgery is often recommended.
5. Failure of Other Treatments: If minimally invasive treatments like rubber band ligation, sclerotherapy, or infrared coagulation have failed to alleviate symptoms, surgery might be considered.
6. Combined Internal and External Hemorrhoids: When both internal and external hemorrhoids are present and symptomatic, surgery might be the most effective treatment option.
Consultation Process
The process of consulting with a specialist for piles surgery involves several steps:
1. Initial Consultation: This usually starts with a visit to a general practitioner or directly to a colorectal surgeon. During this visit, the patient will discuss their symptoms, medical history, and any previous treatments for hemorrhoids.
2. Medical History Review: The specialist will review the patient’s medical history, including any medications, previous medical treatments, and family history of colorectal conditions.
3. Physical Examination: A physical exam will include inspecting the external anal region for external hemorrhoids, skin tags, fissures, or other abnormalities.
4. Digital Rectal Examination (DRE): The specialist may perform a DRE to check for internal hemorrhoidal problems, rectal tumors, or other internal abnormalities.
5. Anoscopy or Proctoscopy: For a more detailed examination, an anoscope or proctoscope – short, rigid, hollow tubes designed for inspecting the anal canal and lower rectum – might be used.
6. Colonoscopy: In some cases, especially if there are concerns about colorectal cancer or inflammatory bowel disease, or if the patient is of an age where colorectal cancer screening is recommended, a colonoscopy may be performed.
7. Discussion of Treatment Options: After the diagnosis, the doctor will discuss the most appropriate treatment options based on the type, severity, and persistence of the hemorrhoids.
8. Informed Consent: If surgery is recommended, the specialist will explain the procedure, including its risks, benefits, and expected recovery process. The patient will have the opportunity to ask questions and will need to give informed consent before proceeding.
9. Pre-operative Preparations: Finally, if surgery is decided upon, the patient will receive instructions for preparing for the surgery, including dietary restrictions, medication adjustments, and bowel preparation requirements.
The decision to proceed with surgery is usually made after careful consideration of the patient’s specific situation, the severity of symptoms, and the response to other treatments. It is essential for patients to fully understand the procedure, its implications, and the recovery process to make an informed decision.
Types of Piles Surgery
Hemorrhoidectomy
A hemorrhoidectomy is a surgical procedure to remove hemorrhoids, typically recommended for severe or large internal or external hemorrhoids, particularly when other treatments have failed.
- Procedure: The surgery involves making incisions in the tissue around the hemorrhoids to remove them. It can be performed under general anesthesia, spinal anesthesia, or a local anesthetic combined with sedation.
- Appropriateness: Best suited for patients with large, prolapsing, or severely bleeding hemorrhoids. It’s often the choice for external hemorrhoids and those that have not responded to other treatments.
- Risks: As with any surgery, there are risks of complications such as bleeding, infection, and reactions to anesthesia. Postoperative pain is a significant concern and can be intense. There’s also a small risk of urinary retention and fecal incontinence.
- Success Rate: Hemorrhoidectomy has a high success rate, with most patients experiencing significant symptom relief.
However, hemorrhoids can recur, especially if the underlying causes (like chronic constipation) are not addressed.
Stapled Hemorrhoidopexy
Also known as stapled hemorrhoidectomy or Procedure for Prolapse and Hemorrhoids (PPH), this is a less invasive option compared to traditional hemorrhoidectomy.
- Procedure: This surgery involves using a special stapling device to reposition and fix the prolapsed hemorrhoids back to their original location within the rectum. The procedure cuts off the blood supply to the hemorrhoids, causing them to shrink.
- Appropriateness: Ideal for patients with prolapsed internal hemorrhoids. Not typically recommended for external hemorrhoids.
- Comparison with Traditional Surgery: It is generally less painful than a conventional hemorrhoidectomy and often allows for a quicker return to normal activities. However, it may have a higher recurrence rate compared to traditional hemorrhoidectomy.
- Risks: Risks include bleeding, severe pain, and in rare cases, rectal perforation. There may also be a risk of recurrence and rectal prolapse.
Laser Surgery
Laser surgery for piles is a newer technique that is becoming more widely available.
- Procedure: The procedure uses a laser to burn and cut the hemorrhoidal tissue. It is precise and causes less damage to the surrounding tissues.
- Benefits: The benefits of laser surgery include less pain, minimal bleeding, and faster recovery compared to traditional surgery. The precision of the laser also allows for the treatment of more complex cases.
- Limitations: Despite these benefits, laser surgery can be more expensive than other surgical options. Additionally, it requires specialized equipment and training. As a newer technique, long-term data on success rates and potential complications are still being gathered.
- Appropriateness: It can be used for both internal and external hemorrhoids, particularly in cases where precision is necessary or where a less invasive procedure is preferred.
Each of these surgical options has its indications, benefits, and risks. The choice of procedure depends on the individual patient’s condition, the severity of the hemorrhoids, and the surgeon’s experience and preference.
It is essential for patients to discuss these options thoroughly with their healthcare provider to understand the best course of action for their specific case.
Preparing for Surgery
Pre-Operative Instructions
Proper preparation before piles surgery can help ensure a smoother procedure and recovery. Here are some general guidelines:
- Diet Adjustments: Patients may be advised to switch to a liquid diet 24-48 hours before surgery to ensure the bowels are empty. This can include broths, juices, and gelatin. Avoiding solid foods helps minimize the risk of complications during the surgery.
- Bowel Preparation: A laxative or an enema may be prescribed the night before or the morning of the surgery to cleanse the intestines. This is important for a clear surgical field and to reduce the risk of infection.
- Medication Management: Patients should inform their surgeon about all medications they are taking, including over-the-counter drugs and supplements. Some medications, particularly those that affect blood clotting like aspirin, warfarin, or certain anti-inflammatory drugs, may need to be stopped or adjusted before surgery.
- Fasting: Typically, patients are required to fast (not eat or drink) for a certain period, usually after midnight, on the day before the surgery. This is to prevent the risk of aspiration during anesthesia.
- Hydration: Good hydration is important before surgery. Patients should drink plenty of water up until the time they are advised to start fasting.
- Smoking and Alcohol: It’s recommended to avoid smoking and consuming alcohol at least 24 hours before surgery as they can affect the body’s ability to heal and respond to anesthesia.
- Physical Health: Maintaining good physical health, including light exercise and sufficient sleep, can aid in a smoother surgery and recovery.
Mental Preparation
Mental readiness is a crucial aspect of preparing for surgery:
- Understanding the Procedure: Patients should have a clear understanding of the surgical procedure, including what to expect during and after the surgery. This can help alleviate fears and anxiety.
- Setting Realistic Expectations: Understanding the likely outcomes, potential risks, and the recovery process helps in mentally preparing for the surgery and the post-operative phase.
- Stress Management: Techniques such as deep breathing, meditation, or speaking with a counselor can be beneficial in managing pre-surgery anxiety.
- Support Systems: Having a support system in place is vital. This can include family, friends, or support groups. Patients should plan for someone to accompany them to the hospital and help with post-surgery care at home.
- Discussing Concerns: Patients should feel free to discuss any fears, anxieties, or concerns with their healthcare provider. Getting answers to all questions can help in feeling more secure and prepared.
- Positive Mindset: Maintaining a positive outlook and focusing on the benefits of the surgery, like relief from symptoms and improved quality of life, can be very beneficial for mental preparation.
Preparing both physically and mentally for piles surgery can help ensure a smoother experience and recovery. It is important for patients to closely follow the specific instructions provided by their healthcare team, as individual requirements may vary.
The Surgical Procedure
Step-by-Step Guide
Walking through the surgical process for piles surgery can provide patients with a clearer picture of what to expect. This step-by-step guide focuses on a general overview of the procedure:
1. Arrival at the Hospital: Patients typically arrive at the hospital on the morning of the surgery. They undergo final pre-operative checks, including vital signs assessment and a review of medical history.
2. Preparation for Surgery: The patient changes into a hospital gown, and an intravenous (IV) line may be started for fluids and medications. The surgical site is then cleaned and prepped.
3. Anesthesia: The type of anesthesia used (general, spinal, or local with sedation) depends on the specific procedure and patient factors. The anesthesiologist administers anesthesia to ensure the patient is comfortable and pain-free during the surgery.
4. Surgical Procedure: The specifics of the procedure vary depending on the type of surgery (hemorrhoidectomy, stapled hemorrhoidopexy, or laser surgery). Generally, the surgeon accesses the hemorrhoids and performs the necessary steps to remove or reposition them. The duration of the surgery can vary, typically lasting from 30 minutes to an hour.
5. Hemostasis: Throughout the procedure, the surgeon ensures that any bleeding is controlled. This is crucial for preventing postoperative complications.
6. Closure and Dressing: Once the hemorrhoids are treated, the surgical area is either stitched or left open (in some hemorrhoidectomy procedures) and then dressed appropriately.
7. Recovery from Anesthesia: After the surgery, the patient is moved to a recovery area where they are closely monitored as they wake up from anesthesia. Vital signs are checked, and pain management begins.
8. Post-Operative Assessment: Once awake, the patient is assessed for any immediate post-operative complications like bleeding or severe pain.
9. Discharge Instructions: If the surgery is done on an outpatient basis, patients are usually allowed to go home the same day. They receive detailed instructions on post-operative care, pain management, signs of complications, and follow-up appointments.
Intra-Operative Care
Ensuring safety and efficacy during the surgical procedure involves several key elements:
1. Monitoring: Continuous monitoring of the patient’s vital signs (heart rate, blood pressure, oxygen saturation) is done to detect any immediate issues that may arise during the surgery.
2. Sterility: Maintaining a sterile environment is crucial to prevent infections. All surgical instruments and the operating field are sterilized, and the surgical team follows strict hygiene protocols.
3. Pain Management: Anesthesiologists manage pain and comfort throughout the procedure. The type and amount of anesthesia are carefully adjusted as needed.
4. Technique Precision: The surgeon uses precise techniques to minimize tissue damage and ensure effective treatment of hemorrhoids. This includes careful dissection, accurate hemostasis, and appropriate tissue handling.
5. Communication: Effective communication among the surgical team members is vital for a successful operation. This includes readiness to handle any unforeseen complications that may arise during the procedure.
6. Documentation: Accurate documentation of the procedure is maintained, including any unusual occurrences or deviations from the standard procedure.
The focus during piles surgery is on patient safety, effective treatment of the hemorrhoids, minimizing complications, and ensuring a smooth recovery process. The surgical team’s expertise and the comprehensive intra-operative care protocols play a crucial role in the success of the surgery.
Recovery and Aftercare
Immediate Post-Operative Care
The period immediately following piles surgery is crucial for recovery and monitoring for any complications:
1. Monitoring: Patients are typically moved to a recovery room where their vital signs (heart rate, blood pressure, oxygen levels) are closely monitored as they come out of anesthesia.
2. Pain Management: One of the first issues addressed post-surgery is pain control. Patients are usually given pain medication either intravenously or through oral medications. The intensity of pain can vary depending on the type of surgery performed.
3. Hydration and Nutrition: Once awake and stable, patients are encouraged to drink fluids. Eating can often resume with light foods as tolerated.
4. Activity: Early mobilization is encouraged to help prevent complications such as blood clots. Patients are usually urged to walk with assistance as soon as they feel able.
5. Wound Care: Instructions on how to care for the surgical area are provided, which may include keeping the area clean and dry, and when to change dressings, if applicable.
6. Discharge Instructions: Before discharge, patients receive detailed instructions regarding diet, pain management, wound care, and activity restrictions. Information on when to schedule a follow-up visit and signs of complications are also provided.
7. Arrangement for Transportation: Since patients cannot drive immediately following surgery due to the effects of anesthesia, arrangements for a ride home need to be made in advance.
Home Recovery
Recovery at home involves several key components:
1. Pain Management: Continue taking prescribed pain medications as directed. Over-the-counter pain relievers may also be recommended.
2. Diet: A high-fiber diet is crucial to prevent constipation and straining during bowel movements. This includes plenty of fruits, vegetables, whole grains, and water.
3. Bowel Movements: Avoiding constipation is key. Stool softeners may be prescribed. It’s important to avoid straining during bowel movements.
4. Sitz Baths: Taking warm sitz baths can help soothe the area and aid in healing. This involves sitting in a few inches of warm water several times a day, especially after bowel movements.
5. Activity Level: Gradually increase activity levels as tolerated. Avoid heavy lifting or strenuous activities for the first few weeks after surgery.
6. Wound Care: Follow the surgeon’s instructions on how to care for the wound. This may include cleaning the anal area after each bowel movement and applying topical medications if prescribed.
7. Follow-up Appointments: Attend all scheduled post-operative appointments for monitoring recovery progress and addressing any concerns.
Complications to Watch Out For
While most recoveries are smooth, it’s important to be aware of signs that may indicate complications:
- Excessive Bleeding: A small amount of bleeding is normal, but heavy bleeding should be reported to the doctor immediately.
- Severe Pain: While some pain is expected, intolerable pain or pain that worsens over time should be evaluated.
- Fever and Chills: These could be signs of an infection.
- Difficulty Urinating: Difficulty or inability to urinate is a potential complication that requires prompt medical attention.
- Unusual Discharge: Any pus or foul-smelling discharge from the surgical site should be reported.
- Swelling: Significant swelling or the formation of large lumps around the anal area should be checked by a doctor.
Patients should seek medical help immediately if they experience any of these symptoms. Prompt attention to complications can prevent more serious outcomes and aid in a smoother recovery.
Long-Term Management and Prevention
Lifestyle Changes
To prevent the recurrence of piles and maintain good colorectal health, several lifestyle and dietary changes are recommended:
1. Dietary Modifications:
- Increase Fiber Intake: A high-fiber diet helps to soften stools and increase their bulk, which can prevent straining during bowel movements. Include more fruits, vegetables, whole grains, and legumes in your diet.
- Stay Hydrated: Drink plenty of water throughout the day to help keep stools soft.
- Limit Certain Foods: Reduce the intake of spicy and processed foods, which can exacerbate hemorrhoid symptoms.
2. Regular Exercise:
- Engage in regular, moderate exercise to help prevent constipation and reduce pressure on the veins in the lower rectum and anus. Activities like walking, swimming, or yoga can be particularly beneficial.
3. Bowel Habits:
- Avoid Straining: Straining during bowel movements increases pressure in the lower rectum, aggravating hemorrhoids.
- Don’t Delay Bowel Movements: Go to the bathroom as soon as you feel the urge to prevent stools from becoming hard and difficult to pass.
4. Weight Management:
- If overweight, working towards a healthier weight can reduce the pressure on the pelvic veins.
5. Avoid Prolonged Sitting:
- Sitting for long periods, especially on the toilet, can increase the pressure on the veins in the anus and rectum.
6. Proper Anal Hygiene:
- Clean the anal area gently after each bowel movement using moist wipes or a bidet instead of dry toilet paper.
Follow-Up Care
Consistent follow-up care is crucial to monitor recovery and prevent complications:
1. Regular Doctor Visits: Schedule and attend follow-up appointments as recommended by your healthcare provider. These visits are essential for monitoring the healing process and ensuring that the hemorrhoids have not recurred.
2. Monitoring Symptoms: Be vigilant about any new or returning symptoms and report them to your doctor immediately. This includes any bleeding, pain, or changes in bowel habits.
3. Long-Term Surveillance: Depending on the severity of your condition and the type of surgery performed, your doctor may recommend periodic check-ups to monitor for any changes or complications.
4. Medication Management: If prescribed any medications post-surgery (such as stool softeners or fiber supplements), use them as directed and discuss any long-term use with your doctor
By incorporating these lifestyle and dietary changes and adhering to follow-up care, individuals can significantly reduce the risk of piles recurrence and maintain overall colorectal health.
The journey through piles surgery and recovery can be challenging, but it is a path towards a more comfortable and healthy life. The advancements in surgical techniques have made these procedures safer and more effective, with shorter recovery times. With the right care, guidance, and lifestyle adjustments, you can look forward to a future with reduced discomfort and improved overall well-being.
Frequently Asked Questions on Piles Surgery
1. What are the signs that I might need piles surgery?
You might need surgery if you experience persistent or severe pain, large hemorrhoids, prolapsed internal hemorrhoids, failure of other treatments, or complications like significant bleeding.
2. How long does piles surgery typically take?
The duration of piles surgery can vary but generally lasts between 30 minutes to an hour, depending on the type of procedure and complexity of the case.
3. What are the risks associated with piles surgery?
Common risks include pain, bleeding, infection, and reactions to anesthesia. Specific procedures may have unique risks, such as urinary retention or fecal incontinence for hemorrhoidectomy, and rectal perforation for stapled hemorrhoidopexy.
4. What type of anesthesia is used during piles surgery?
Anesthesia type can vary from local with sedation, spinal, to general anesthesia, depending on the procedure and patient factors.
5. How painful is the recovery from piles surgery?
Post-operative pain is expected, especially with traditional hemorrhoidectomy, but can be managed with prescribed pain medications. The intensity of pain gradually decreases over a few days to a week.
6. How long is the recovery period after piles surgery?
Recovery can vary but generally, patients can return to normal activities within a few days to a week, with complete healing taking a few weeks to a couple of months.
7. When can I return to work after undergoing piles surgery?
Depending on the nature of your job, you may return to work in a few days to a week, but you should avoid strenuous activities for a few weeks post-surgery.
8. What dietary changes should I make after piles surgery?
A high-fiber diet with plenty of fluids is recommended to prevent constipation and ensure smooth bowel movements. Avoid spicy and processed foods during the recovery period.
9. Will piles recur after surgery?
While surgery is effective, hemorrhoids can recur, especially if the underlying causes like chronic constipation or prolonged sitting are not addressed. Lifestyle changes can help reduce the risk of recurrence.
10. Can I manage piles without surgery?
Many piles can be managed with lifestyle changes, dietary adjustments, and non-surgical treatments. Surgery is usually recommended for severe or persistent cases.
11. What are the alternatives to piles surgery?
Alternatives include non-surgical treatments like rubber band ligation, sclerotherapy, and infrared coagulation, which are less invasive and suitable for certain types of hemorrhoids.
12. How do I take care of the surgical area after piles surgery?
Keep the area clean and dry, use a sitz bath for comfort, avoid straining during bowel movements, and follow any specific wound care instructions given by your doctor.
13. What should I do if I experience complications after piles surgery?
Contact your doctor immediately if you experience excessive bleeding, severe pain, fever, difficulty in urinating, or any signs of infection.